It’s soul crushing when you find out you’re pregnant only to be told, a few months, weeks or days later, that the pregnancy isn’t viable. A common reason a pregnancy ends early and one that is very rarely discussed is an ectopic pregnancy.
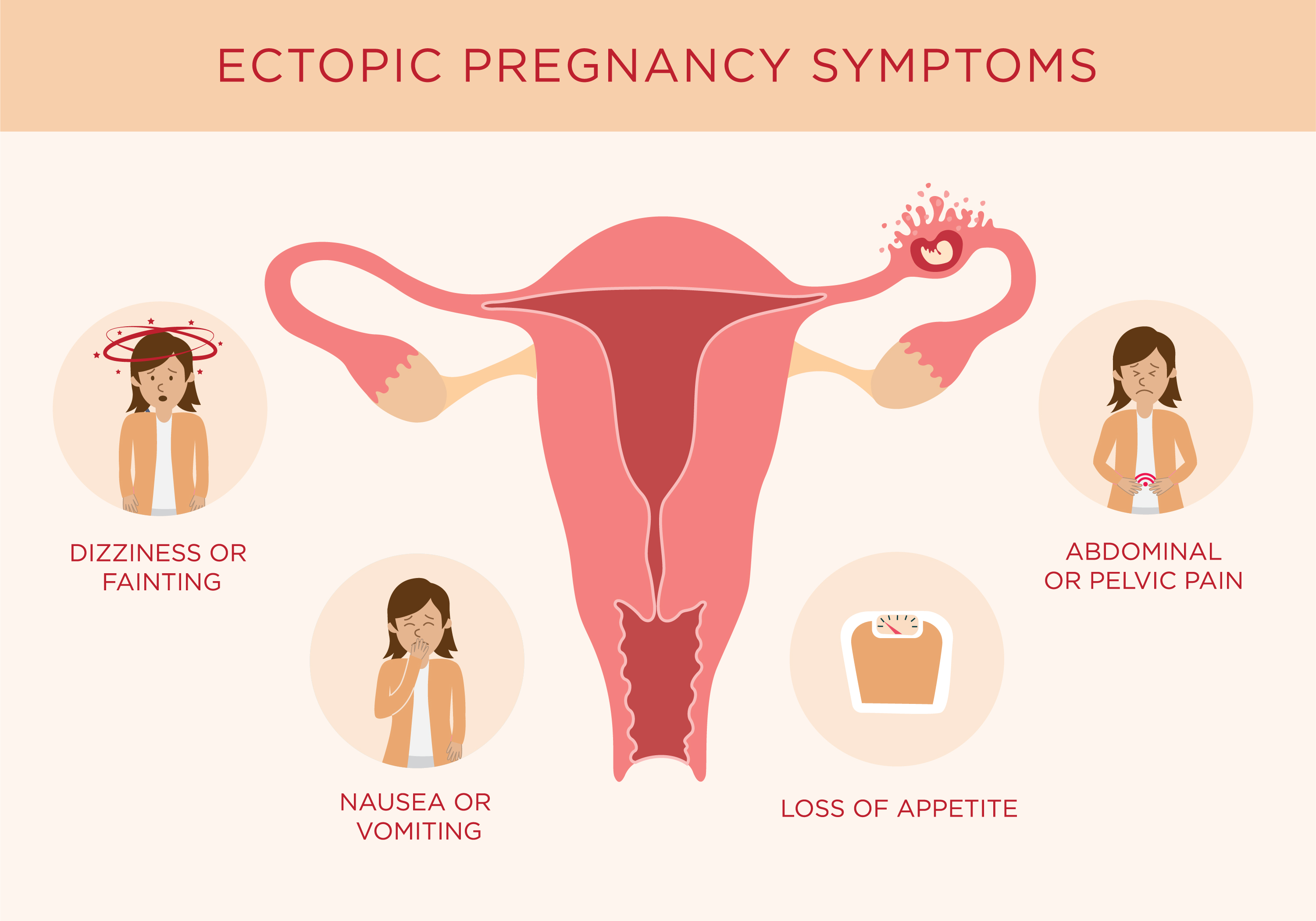
“An ectopic pregnancy is a pregnancy that implants in the wrong location – anywhere other than the top part of the cavity within the uterus,” says Dr Lucky Sekhon, OBGYN and reproductive endocrinologist. “The most common location for an ectopic pregnancy is the fallopian tubes, the pathway between the ovaries and the uterus where fertilization of the egg with sperm takes place. Ectopic pregnancies can also be found in the cervix, on the ovaries, in the abdominal or pelvic cavity, and even at the junction between the uterine cavity and the opening of a fallopian tube. Because ectopic pregnancies implant in locations not meant to support a growing pregnancy, they often result in spontaneous miscarriage where the pregnancy stops developing due to lack of blood supply which starves the pregnancy of essential nutrients and oxygen. If a pregnancy continues to grow or begins to bleed due to miscarriage, it can stretch the surrounding structure (ie. fallopian tube) and cause it to rupture, which can lead to rapid blood loss and a potentially life threatening emergency if the bleeding is not recognized and stopped in a timely fashion.”
What are the risk factors for an ectopic pregnancy?
According to Dr. Sekhon The most prominent risk factor for an ectopic pregnancy, especially for a tubal ectopic pregnancy, is a history of pelvic infection. “Prior infections and sexually transmitted diseases, such as gonorrhea and chlamydia, which often go unrecognized at time of infection, can silently lead to scarring of the fallopian tubes which can predispose an individual to ectopic pregnancy.” Another major risk factor, she says, is a gynecologic condition called endometriosis, where the lining of the uterus is found in locations outside of the uterus, causing scar tissue formation and pelvic pain over time.
As if women suffering from fertility problems don’t have it hard enough, undergoing fertility treatments, which lead to the release of multiple eggs during ovulation, is also an independent risk factor for an ectopic pregnancy as the statistical odds of an abnormal implantation increases with the number of potential eggs available for fertilization and eventually implantation as a pregnancy. “Having a history of prior ectopic pregnancy is thought to confer a ~25% risk of recurrence in future pregnancy,” says Dr. Sekhon. “The reason behind this high recurrence rate, is that the underlying cause of the first ectopic pregnancy would still be a risk factor for future pregnancies. Also, the initial ectopic pregnancy could cause further scarring and damage of the fallopian tube, increasing the risk of future ectopic if ovulation occurs on that same side.”
Ectopic pregnancies are usually discovered in the first few weeks of pregnancy. “If during early pregnancy (ie. within two weeks since missing one’s period), the pregnancy can not be visualized inside the uterine cavity on pelvic ultrasound, this is usually the first sign that there could be an ectopic pregnancy,” says Dr. Sekhon. That said, not seeing a pregnancy inside the uterus on ultrasound could also mean that the ultrasound is being done too early (before pregnancy can be detected on imaging) or that the pregnancy is abnormal and stopped developing in the uterus as it should (a miscarriage). “The only way to rule this out is to do follow up blood work to assess whether the pregnancy hormone, bHCG (beta human chorionic gonadotropin) is rising and whether a pregnancy ultimately appears inside the uterus – and if not, if it can be seen in an ectopic location (ie. in the tube or pelvic cavity).”
What happens after an ectopic diagnoses?
If an ectopic pregnancy is diagnosed and localized, it can be treated either medically or surgically. “Medical treatment of an ectopic pregnancy involved a medication called methotrexate, which is a chemotherapeutic drug that can be used at a lower dose and in a single or multi-dose protocol,” says Dr. Sekhon. “It works by stopping cells’ ability to replicate and divide and this tends to impact the fastest growing cells the most, which works effectively to target an early pregnancy. It’s administered as an intramuscular injection. Because it can linger in one’s system for weeks to months, and is toxic to a growing pregnancy, it is important to avoid pregnancy for three months post injection.”
If methotrexate cannot be given because of a drug allergy or underlying medical issues which make methotrexate an unsafe choice, the ectopic pregnancy can be surgically excised. “This is the only treatment option if the ectopic pregnancy is far gone enough that it has caused rupture and uncontrolled bleeding. If the ectopic pregnancy is found in the fallopian tube, the entire tube could be removed or in some instances, where much of the tube’s normal anatomy is preserved, there could be a role for a more conservative surgical approach whereby the tube is spared and only the ectopic itself is removed by making a small incision in the tube.”
Is there a way to prevent an ectopic pregnancy?
Before diving into prevention, it’s important to underline that it’s crucial to see your doctor early on when you discover you’re pregnant as early detection is key to best treat an ectopic pregnancy. “You can prevent having a complicated (ie. ruptured and requiring emergency surgery) ectopic pregnancy with early diagnosis and intervention,” says Dr. Sekhon. “This means seeing one’s doctor as soon as you become pregnant so that you can be followed along closely and an ectopic pregnancy can be diagnosed as early as possible.”
As far as preventing an ectopic pregnancy before it happens, Dr. Sekhon says that patients can prevent the major risk factor of pelvic infections by practicing safe sex and using condoms to lower the risk of contracting infections such as gonorrhea or chlamydia. “If you are known to have a blocked fallopian tube (something that may be discovered with a hysterosalpingogram – an X-ray of the pelvic after having dye injected into the cervix in order to fill the fallopian tubes and assess them for damage and blockages), you should avoid moving forward with treatments or pregnancy attempts on months you happen to only be ovulating on the blocked side.”






